Muscular System Diseases
The Muscular System
In addition to muscles, the muscular system consists of nervous and connective tissue. The muscular system's most obvious task is to enable movement in the body, which it does by receiving electrical impulses from the brain. This movement can range from running to blinking your eyes. Muscles make up 40% of the body's total weight, and because of their mass they are the body's main source of heat generation. Muscles also help to regulate the body's temperature, keeping it constant. The muscular system is so complex in its connections that one affected muscle could cause repercussions for the entire system.[Read more: Muscular System Diseases | eHow.com http://www.ehow.com/about_5389470_diseases-muscular-system.html#ixzz2CkbauyAt]
Atony vs. Atrophy
Atony and atrophy are two general types of conditions that can develop from a muscular system disease. Atony refers to a state in which muscles no longer maintain their normal elasticity and become floppy. Atrophy refers to a state where muscle tissue wastes away, each muscle fiber shrinking in size. This can be caused by muscle disuse or when nerve impulses become ineffective.[Read more: Muscular System Diseases | eHow.com http://www.ehow.com/about_5389470_diseases-muscular-system.html#ixzz2Ckcf96Sp]Muscular Dystrophy
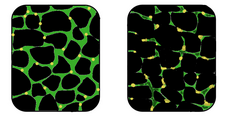
In affected muscle the tissue becomes disorganized and the concentration of dystrophin (green) is greatly reduced.
[From: http://en.wikipedia.org/wiki/Muscular_dystrophy]
Muscular dystrophy, or MD, is an inherited muscle disease that causes muscle fibers to become incredibly susceptible to harm. Muscles grow progressively weaker, and muscle fiber is replaced with fat and other tissue. Symptoms include lack of coordination, muscle weakness, and a progressive loss of mobility.
[Read more: Muscular System Diseases | eHow.com http://www.ehow.com/about_5389470_diseases-muscular-system.html#ixzz2CkeZPzUe]
Diagnosis
A physical examination and the patient's medical history will help the doctor determine the type of muscular dystrophy. Specific muscle groups are affected by different types of muscular dystrophy.
Often, there is a loss of muscle mass (wasting), which may be hard to see because some types of muscular dystrophy cause a build up of fat and connective tissue that makes the muscle appear larger. This is called pseudohypertrophy.
[From: http://en.wikipedia.org/wiki/Muscular_dystrophy#Diagnosis]
Duchenne Muscular Dystrophy
 |
| Histopathology of gastrocnemius muscle from patient who died of pseudohypertrophic muscular dystrophy, Duchenne type. Cross section of muscle shows extensive replacement of muscle fibers by adipose cells. [From: http://en.wikipedia.org/wiki/Duchenne_muscular_dystrophy] |
Duchenne muscular dystrophy (DMD) is a recessive X-linked form of muscular dystrophy, affecting around 1 in 3,600 boys, which results in muscle degeneration and eventual death. The disorder is caused by a mutation in the dystrophin gene, located on the human X chromosome, which codes for the protein dystrophin, an important structural component within muscle tissue that provides structural stability to the dystroglycan complex (DGC) of the cell membrane. While both sexes can carry the mutation, females rarely exhibit signs of the disease.
Symptoms usually appear in male children before age 5 and may be visible in early infancy. Even though symptoms do not appear until early infancy, there is laboratory evidence, which can distinguish a child with the disease at birth. Progressive proximal muscle weakness of the legs and pelvis associated with a loss of muscle mass is observed first. Eventually this weakness spreads to the arms, neck, and other areas. Early signs may include pseudohypertrophy (enlargement of calf and deltoid muscles), low endurance, and difficulties in standing unaided or inability to ascend staircases. As the condition progresses, muscle tissue experiences wasting and is eventually replaced by fat and fibrotic tissue (fibrosis). By age 10, braces may be required to aid in walking but most patients are wheelchair dependent by age 12. Later symptoms may include abnormal bone development that lead to skeletal deformities, including curvature of the spine. Due to progressive deterioration of muscle, loss of movement occurs, eventually leading to paralysis. Intellectual impairment may or may not be present but if present, does not progressively worsen as the child ages. The average life expectancy for patients afflicted with DMD is around 25. [From: http://en.wikipedia.org/wiki/Duchenne_muscular_dystrophy]
Diagnosis
If a person has weak muscles that become weaker over time, they may have muscular dystrophy. High levels of a chemical calledcreatine kinase (CPK) found in the blood may also help diagnose muscular dystrophy. High levels of creatine kinase don't give a definite diagnosis, since many other muscle diseases can also cause this.Testing for very low levels of dystrophin in the muscles can also be used to diagnose Duchenne muscular dystrophy. For other types of muscular dystrophy, specific blood tests can be done to help your doctor determine which type of muscular dystrophy you have.A test called an electromyogram (EMG) involves passing tiny electrical shocks through the muscles. It can be performed to test whether the muscles and nerves are working properly.A muscle biopsy may also be used to help with diagnosis. In this procedure, a doctor surgically removes a small piece or sample of the muscle and looks at it under the microscope. A muscle with muscular dystrophy has many dead and abnormally large muscle fibres. As the disease progresses, the dead muscle is replaced with fat and other kinds of tissue.[From: http://chealth.canoe.ca/condition_info_details.asp?channel_id=0&relation_id=0&disease_id=91&page_no=2]Myasthenia Gravis

Diagnosis
[Read more: http://www.chop.edu/healthinfo/myasthenia-gravis-1.html]
Motor neurons are nerve cells located in the brain, brainstem, and spinal cord that serve as controlling units and vital communication links between the nervous system and the voluntary muscles of the body. Messages from motor neurons in the brain (called upper motor neurons) are transmitted to motor neurons in the spinal cord (called lower motor neurons) and from them to particular muscles. In ALS, both the upper motor neurons and the lower motor neurons degenerate or die, ceasing to send messages to muscles. Unable to function, the muscles gradually weaken, waste away (atrophy), and twitch (fasciculations) . Eventually, the ability of the brain to start and control voluntary movement is lost.
ALS causes weakness with a wide range of disabilities (see section titled "What are the symptoms?"). Eventually, all muscles under voluntary control are affected, and patients lose their strength and the ability to move their arms, legs, and body. When muscles in the diaphragm and chest wall fail, patients lose the ability to breathe without ventilatory support. Most people with ALS die from respiratory failure, usually within 3 to 5 years from the onset of symptoms. However, about 10 percent of ALS patients survive for 10 or more years.
Although the disease usually does not impair a person's mind or intelligence, several recent studies suggest that some ALS patients may have alterations in cognitive functions such as depression and problems with decision-making and memory.
ALS does not affect a person's ability to see, smell, taste, hear, or recognize touch. Patients usually maintain control of eye muscles and bladder and bowel functions, although in the late stages of the disease most patients will need help getting to and from the bathroom.
ALS
Amyotrophic lateral sclerosis (ALS), sometimes called Lou Gehrig's disease, is a rapidly progressive, invariably fatal neurological disease that attacks the nerve cells (neurons) responsible for controlling voluntary muscles. The disease belongs to a group of disorders known as motor neuron diseases, which are characterized by the gradual degeneration and death of motor neurons.Motor neurons are nerve cells located in the brain, brainstem, and spinal cord that serve as controlling units and vital communication links between the nervous system and the voluntary muscles of the body. Messages from motor neurons in the brain (called upper motor neurons) are transmitted to motor neurons in the spinal cord (called lower motor neurons) and from them to particular muscles. In ALS, both the upper motor neurons and the lower motor neurons degenerate or die, ceasing to send messages to muscles. Unable to function, the muscles gradually weaken, waste away (atrophy), and twitch (fasciculations) . Eventually, the ability of the brain to start and control voluntary movement is lost.
ALS causes weakness with a wide range of disabilities (see section titled "What are the symptoms?"). Eventually, all muscles under voluntary control are affected, and patients lose their strength and the ability to move their arms, legs, and body. When muscles in the diaphragm and chest wall fail, patients lose the ability to breathe without ventilatory support. Most people with ALS die from respiratory failure, usually within 3 to 5 years from the onset of symptoms. However, about 10 percent of ALS patients survive for 10 or more years.
Although the disease usually does not impair a person's mind or intelligence, several recent studies suggest that some ALS patients may have alterations in cognitive functions such as depression and problems with decision-making and memory.
ALS does not affect a person's ability to see, smell, taste, hear, or recognize touch. Patients usually maintain control of eye muscles and bladder and bowel functions, although in the late stages of the disease most patients will need help getting to and from the bathroom.
[Read more: http://www.ninds.nih.gov/disorders/amyotrophiclateralsclerosis/detail_ALS.htm]
Diagnosis
No one test can provide a definitive diagnosis of ALS, although the presence of upper and lower motor neuron signs in a single limb is strongly suggestive. Instead, the diagnosis of ALS is primarily based on the symptoms and signs the physician observes in the patient and a series of tests to rule out other diseases. Physicians obtain the patient's full medical history and usually conduct a neurologic examination at regular intervals to assess whether symptoms such as muscle weakness, atrophy of muscles, hyperreflexia, and spasticity are getting progressively worse.Cerebral Palsy
There are several different types of cerebral palsy, including spastic, dyskinetic, ataxic, hypotonic, and mixed.
Cerebral palsy is caused by injuries or abnormalities of the brain. Most of these problems occur as the baby grows in the womb, but they can happen at any time during the first 2 years of life, while the baby's brain is still developing.
In some people with cerebral palsy, parts of the brain are injured due to low levels of oxygen (hypoxia) in the area. It is not known why this occurs.
Premature infants have a slightly higher risk of developing cerebral palsy. Cerebral palsy may also occur during early infancy as a result of several conditions, including:
Bleeding in the brain
Brain infections (encephalitis, meningitis, herpes simplex infections)
Head injury
Infections in the mother during pregnancy (rubella)
Severe jaundice
In some cases the cause of cerebral palsy is never determined.
[Read more: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001734/]
Diagnosis
In severe cases, the child may be diagnosed soon after birth, but for the majority, diagnosis can be made in the first two years.
For those with milder symptoms, a diagnosis may not be rendered until the brain is fully developed at three to five years of age. For example, the average age of diagnosis for a child with spastic diplegia, a very common form of cerebral palsy, is 18 months.
This can be a difficult time for parents who suspect something might be different about their child. Often, parents are first to notice their child has missed one of the age-appropriate developmental milestones.
If a growth factor is delayed, parents may hope their child is just a slow starter who will “catch up.” While this may be the case, parents should inform the child’s doctor of concerns, nonetheless.
Confirming cerebral palsy can involve many steps. The first is monitoring for key indicators such as:
When does the child reach development milestones and growth chart standards for height and weight?
How do the child’s reflexes react?
Does it seem as if the child is able to focus on and hear his or her caregivers?
Does posture and movement seem abnormal? Doctors will test reflexes, muscle tone, posture, coordination and other factors, all of which can develop over months or even years. Primary care physicians may want to consult medical specialists, or order tests such as MRIs, cranial ultrasounds, or CT scans to obtain an image of the brain. Even once a diagnosis of cerebral palsy is made, parents may wish to seek a second opinion to rule out misdiagnosis.
[From: http://cerebralpalsy.org/about-cerebral-palsy/diagnosis/]